Be yourself; Everyone else is already taken.
— Oscar Wilde.
This is the first post on my new blog. I’m just getting this new blog going, so stay tuned for more. Subscribe below to get notified when I post new updates.
Be yourself; Everyone else is already taken.
— Oscar Wilde.
This is the first post on my new blog. I’m just getting this new blog going, so stay tuned for more. Subscribe below to get notified when I post new updates.
Ha! Trick question! Everyone experiences anxiety at one point or another; it’s a part of being alive. As annoying as it may be, anxiety plays an important role in keeping us safe, and motivating us to get things done. For example, I’ve been putting off writing this blog for days, and the only reason I’m writing it now is because of the impending sense of failure and uselessness I feel whenever I think of potentially failing yet another semi-impulsive endeavor (Ok, maybe that’s a bit extreme, but you get my point). Anxiety motivates us to get important tasks done, whether it’s going to work, doing laundry, or just getting out of bed every day. It’s also super important when it comes to keeping us alive. Anxiety is sort of a way for our body to prepare for fight-or-flight without actually triggering a full-on panic response (yet). Common symptoms of anxiety include:
Personally, I experience… all of these. But it’s important to remember that these symptoms are normal and healthy, so long as they occur in appropriate situations and don’t affect your every-day functioning.
We venture into the realm of anxiety disorders when the effects of anxiety begin to interfere with daily life. For example, it’s normal to feel anxious before a test at school. Maybe you cram in some late-night study sessions, talk to friends about the material, and experience some physical symptoms. But you’re able to go to school and take the test with relative success. What’s NOT normal is being physically ill for days before and after the test, not be able to sleep because you can’t stop worrying about not just the test, but everything, and panic so badly you miss school, fail the test because your mind is racing, and/or get sent home due to an anxiety/panic attack. As examples of unhealthy anxiety go, this is a pretty common example. For me, some of the earliest indicators that I had an anxiety disorder were being unable to even begin to attempt timed math tests (Ah, Mad Minutes. The bane of my elementary school existence), and erasing holes in papers that I made a minor mistake on (like, if I didn’t like the way I had written a certain letter, it would be game over for both that piece of paper and the assignment as a whole). My memories of this period of my life are foggy, but I do have vague memories of tightness in my chest, a frequently upset stomach, and a constant irritability that would quickly escalate into hitting myself and/or throwing things.
There are many different mental conditions that fall under the umbrella of “anxiety disorders”. It is possible to have one of these disorders, all of them, or any variation thereof. Some disorders are only diagnosed after what is considered a less-severe condition intensifies, and others can occur at the same time. The 5 major subsets of anxiety disorders are
Along with an official diagnosis of GAD and OCD, I’ve also experienced symptoms of panic disorder and social anxiety disorder. Many of the symptoms of these disorders overlap and blend together, which is part of why they are all classified as “Anxiety Disorders”. Some of these subcategories have their own, even more specific diagnoses as well.
It’s important to remember that to be diagnosed with any of these disorders, a person has to be experiencing symptoms frequently, and those symptoms have to be interfering with the person’s functioning in every day life. Many of these symptoms on their own are normal and healthy, and not a reason to worry. If you do have any concerns, please go see a medical professional.
Some people who are diagnosed with one or more of these disorders are only in treatment for them for a short period of time, and others for their whole lives. No matter how long or how severely a person is affected, their feelings and struggles are valid and deserving of compassion. There is no one way of having a disorder that makes it more real than another. Some people develop anxiety issues due to trauma, others are born with a chemical imbalance. No matter how someone comes to have an anxiety disorder, we are all in a similar boat with a similar struggle, and nothing can discount that. We all need love, compassion, and patience as we figure out how to function.
There have been many times that I’ve needed to be told to suck it up and push through; that I literally could not afford to let my anxiety stop me from doing what needed to get done. But there have been just as many times, if not more, that I needed to hear that it was ok to feel the way I did, and that it was ok to take care of myself first and listen to what my body and mind were telling me. Even if what I was feeling was irrational, it was still valid, and I wasn’t crazy or wrong for feeling it. It is incredibly frustrating to know that what I’m thinking and feeling is irrational, and still not have any control over it. It’s infuriating to feel symptoms of anxiety come on right as I’m trying to get something done, or even better, when nothing is happening at all to trigger an attack. The last thing I need is to be told that I’m being irrational and I have no reason to feel the way I am. I KNOW that, and I’m trying. And I bet I’m not the only one who feels that way. What I, and many others with anxiety disorders need, is patience and support to help us feel less like a burden, and more like a valued part of our friend’s and family’s lives.
In a future post, I will be talking about different coping techniques and which ones I personally used, so keep an eye out for that. For now, be patient, be compassionate, and be strong.
Thanks for reading, I’ll be back soon.
Ah, the human brain. Even the most normal example of a human being can attest to it’s unreliability and penchant to stop working at the most inopportune moments, but for some of us it’s inability to properly transmit signals and produce chemicals makes our lives even harder than most. Luckily we have handy-dandy neuroscience to help explain why, when we are already late to a lunch meeting, some of our brains decide that tapping EXACTLY 32 times on the doorknob is the most important thing we could be doing (yes, I’ve done that and yes, the people I was meeting were irritated).
While many imaging studies have been done comparing the brains of neurotypical people against those of people with OCD, very little conclusive data have been gathered (because of course not). Luckily, there have been enough consistencies that some theories have been developed. I’ve linked the studies I’m referencing below, if you’d like to read them in their entirety, but I’ve taken what I consider the most pertinent information and condensed it into what I hope is a more decipherable read. In this particular post, I’ll be focusing on the physical size and structure of different areas of the brain, and how that may impact a person’s likelihood of having OCD. I’ll cover chemical imbalances in a later post.
Let’s get sciency.
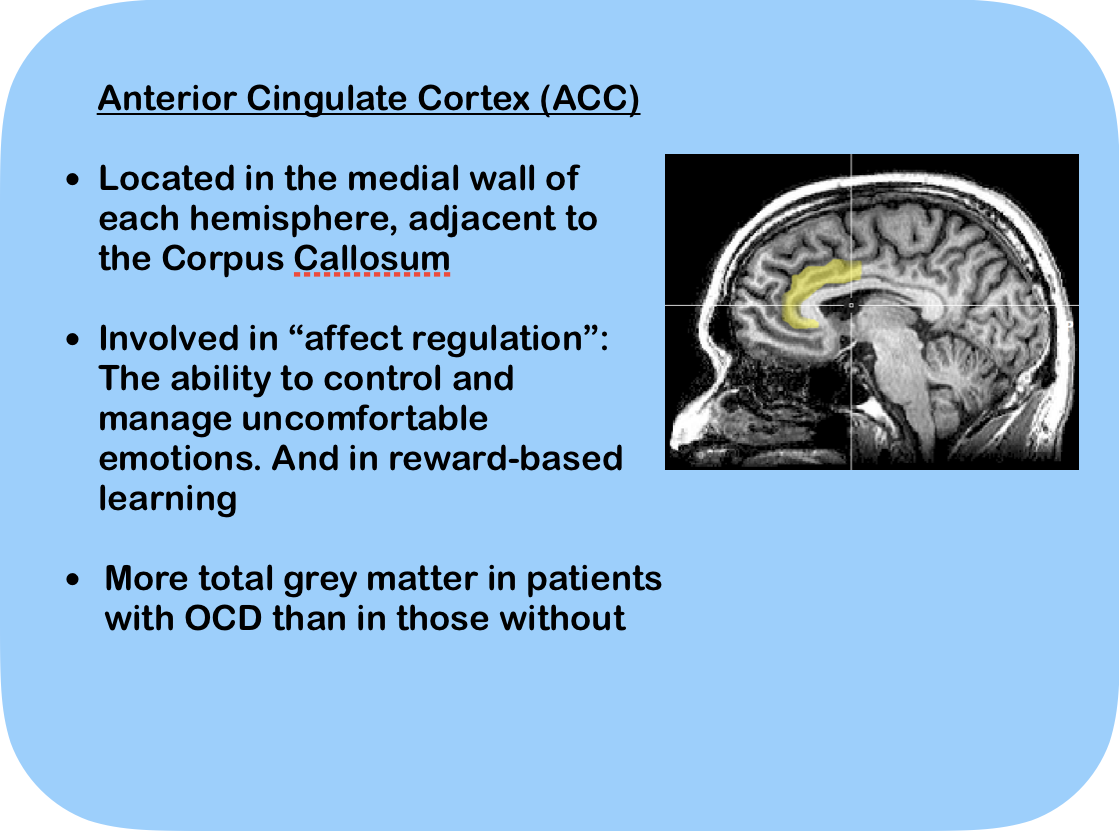
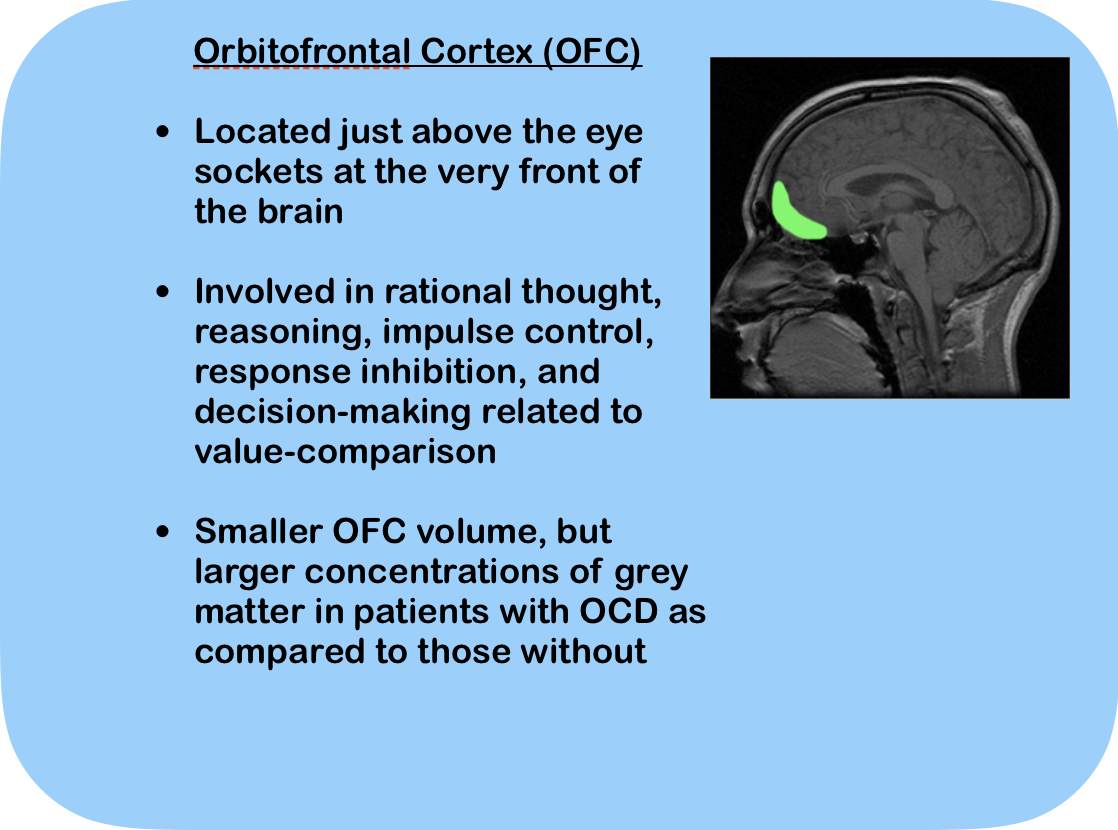
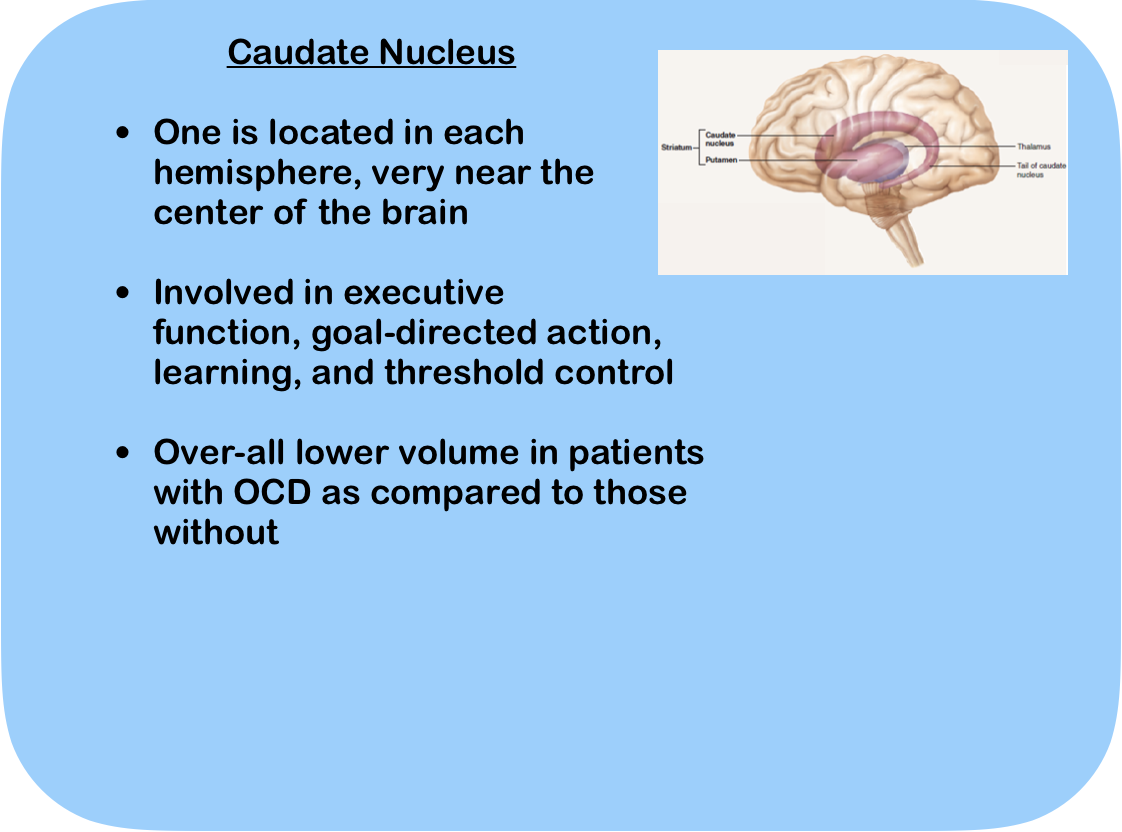
The three areas of the brain that seem to have the most impact when it comes to a person having (or not having) OCD are the Anterior Cingulate Cortex, the Orbitofrontal Cortex, and the Caudare Nucleus. Below are those areas of the brain with a description of it’s location, primary functions, and structural difference between those with OCD and those without.
To begin to understand how these areas and their structures contribute to OCD, we need a little bit more information about grey matter. Grey matter is a part of the central nervous system (CNS) and contains most of the neuronal cell bodies in the CNS. To put it simply, the grey matter is where the “events” of thought, learning, and intelligence occur, and is responsible for memory, emotions, decision making, and self-control (amongst other things, but we have enough to think about as it is).
In the ACC, there is more total grey matter in people with OCD, meaning there are more neuronal cell bodies and more “events” occurring. In an area that is responsible for dealing with uncomfortable emotions, an increased amount of work going on is a strong indicator of OCD, or at least some sort of mental illness. But is this a cause, or an effect? Scientists still aren’t sure, because as we’ve already established, the human brain is complicated and unpredictable (and dumb. But I doubt we’ll get a scientific article on how dumb the human brain is).
Humans have the most developed OFC of any other known organism, but what does it mean when a person’s OFC is smaller than average? While it probably doesn’t mean that we’re devolving into primates, it can theoretically have an impact on how that area of the brain functions (again, there’s never been a definitive conclusion, so much of this information consists of theories and educated guesses. What are scientists even for, anyways?). Despite it’s smaller volume, the OFC also has increased concentrations of grey matter, which implies that there’s still more going on in this area even though there’s less room. In an area of the brain responsible for impulse control, how could these changes affect a person’s thinking and behavior? It is possible that even with more ‘events’ occurring in this area due to increased grey matter, it’s harder for the brain to separate rational thought from irrational and regulate impulses due to it’s smaller-than-average volume? The world may never know.
The Caudate Nucleus is different from the other two areas that we’ve looked at because there’s actually one in each hemisphere of the brain. Most scholarly articles about the Caudate Nuclei describe them as “C” shaped, but I think they look more like tadpoles, or something a little less SFW, but I digress. Overall, the Caudate Nucleus is smaller in people diagnosed with OCD than it is in people without the disorder, implying that there is reduced or limited function. Limited function in the Caudate Nucleus would mean limited goal-directed action, which could be a vital part of the development of OCD.
So what does all this nonsense mean? OCD consists of a complicated mix of impulses, irrational thinking, and decision making. Reward-based learning is involved as well when we consider that people with OCD are rewarded whenever they engage in a compulsion, as their anxiety is temporarily eased. All of these areas of the brain are involved in the feelings and behaviors associated with OCD, and all of these areas have notable differences between those with OCD and those without. And while there may be no definitive conclusions to be drawn from the data that we have, there are certainly some clues as to why our brains work differently. And remember, the human brain is dumb, and I’ve done some postulating and educated guessing in this blog post. So don’t cite me, bro.
Thanks for reading, I’ll be back soon.
Sources:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4476073/
https://neuroscientificallychallenged.com/blog/know-your-brain-orbitofrontal-cortex
https://neuro.psychiatryonline.org/doi/full/10.1176/jnp.23.2.jnp121
“I’m so OCD!”
“I can’t stand having stuff on the counter, I must be OCD.”
“Oh my god, you’re OCD? Can you come clean my house?”
These are all things that have been said to me or in front of me by people who I consider friends and colleagues. And while there has never been any malice behind these words, I always feel a pang of unease whenever I hear them, because with those words comes a stigma and stereotype that completely undermines all the struggle and hard work I have gone through to get to where I am now.
I have Obsessive Compulsive Disorder, and no, I don’t want to clean your house.
You probably wouldn’t want me to anyway, since the only time I ever remember to vacuum the carpet is when I spill something and only God knows when the last time I actually cleaned the bathroom mirrors was. You see, cleaning is not a compulsion that generally accompanies my OCD symptoms. I usually get tics (finger tapping, flinching, swallowing, etc.) and repetitive behaviors. Often times I don’t even get compulsions, just obsessive thoughts that cycle over and over and over and ove-
I might have lost you there. OCD is a very complex and difficult disorder to talk about when both parties don’t understand what it really entails. Let’s break it down.
OCD is a chronic and fairly common disorder that affects roughly 2.3 percent of the population. It’s characterized by a person having uncontrollable, reoccurring thoughts (obsessions) and behaviors (compulsions) that he or she feels the need to repeat over and over. What happens is the brain latches on to a distressing thought and repeats it constantly, triggering an anxiety response. The brain then tries to counteract the anxiety by engaging in a behavior or thought pattern that is thought to negate the distressing thought. So the obsession (the distressing, repetitive thought) leads to a compulsion (behavior thought to negate the obsession). So, for example, one of my obsessions is that someone will break into the house. The compulsion that goes along with this thought is to check, double-check, and triple check that all the doors and windows in the house are locked.
That particular thought is not abnormal for people even without OCD. Plenty of people get in their car, can’t remember if they’ve locked the front door or not, and get out to check before leaving. This behavior crosses the line into OCD territory when the thought that the door might be unlocked causes significant anxiety, and going back and checking the door only once isn’t enough to ease that anxiety. I have been stuck standing at the front door for upwards of 20 minutes before, unlocking and re-locking the door and tugging at the handle to make sure that it’s actually locked. I have been late to lunch with friends, missed appointments, and worked myself into full-blown panic attacks trying to satisfy my OCD. That is OCD. It’s when these obsessions and compulsions start to negatively affect your every-day life.
It’s entirely possible for someone with OCD to have obsessions without compulsions and vice-versa. As I mentioned earlier, I often get obsessive thoughts that don’t come with a compulsion. The thought just circulates over and over in my head and I have to try to deal with it without creating a new compulsive behavior. When this happens, it’s generally an embarrassing or unpleasant memory that gets stuck in my head and I have to use some tricks I learned in therapy to break the cycle. I also have compulsions that seemingly come out of nowhere. One of my early compulsions (that I’ve since conquered) was to make sure NOTHING was within an inch of the edge of my bathroom counter. This was a particularly strong compulsion that would make me get out of bed multiple times a night to make sure there was nothing near the edge of the counter. There were nights where I would still be awake at 3 am because I couldn’t quiet that particular compulsion, even when nothing was anywhere near the edge. It was frustrating, because I knew that what I was doing was illogical. I knew that it didn’t matter where things were on the counter, and that I needed to go to sleep, but the compulsion was so strong that I couldn’t fight it, and it was just easier to stay up late to keep checking the counter than it was to try and fight it and sleep.
So we have obsessions, we have compulsions, and we have OCD. We have a disorder that can be severely disruptive to people’s lives. And we have people who make comments like, “Oh, your house must be spotless! I’m so jealous.”
Yes, some people with OCD are obsessive cleaners/organizers. But they don’t enjoy cleaning. One of the most defining parts of OCD is that sufferers do not get any satisfaction or joy when engaging in a compulsion other than a small (and often very temporary) relief from their anxiety. When it comes to cleaning as a compulsion, often times the person cleans far beyond what would be considered normal housekeeping. It can consume hours of each and every day, and become a huge hinderance in personal relationships, work, and hobbies. People who are obsessive-compulsive cleaners are not any more “lucky” than someone who obsessively checks their locks.
I know that people don’t mean anything when they say things like, “I’m so OCD,” but I think that’s the problem (not to mention that saying “I’m so Obsessive Compulsive Disorder” doesn’t make ANY sense). Phrases like, “Don’t be so bipolar,” “That’s retarded,” and, “You’re OCD about your kitchen,” all contribute to the stigma and misinformation about these disorders, and belittle those who actually suffer from them. It’s not that difficult to say, “You’re being really anal retentive about your kitchen,” and it helps protect those who suffer from a real and problematic disorder (you also get some bonus potty-humor if you roll that way). Find different words, expand your vocabulary, and educate yourself about the words you use. Just the fact that you read this post means that you’re curious and interested in learning more about OCD, and I hope that I’ve helped shed some light on the disorder and expanded your understanding of what people with OCD really experience in their every day lives.
Thanks for reading, I’ll be back soon.